Seasonal flu recognizes the symptoms.
Seasonal influenza is an acute respiratory infection caused by influenza viruses that circulate in all parts of the world.
There are 4 types of seasonal influenza viruses, types A, B, C, and D. Influenza A and B viruses circulate and cause seasonal epidemics of disease.
- Influenza A viruses are further classified into subtypes according to the combinations of the hemagglutinin (HA) and the neuraminidase (NA), the proteins on the surface of the virus. Currently circulating in humans are subtype A(H1N1) and A(H3N2) influenza viruses. The A(H1N1) is also written as A(H1N1)pdm09 as it caused the pandemic in 2009 and subsequently replaced the seasonal influenza A(H1N1) virus which had circulated before 2009. Only influenza-type A viruses are known to have caused pandemics.
- Influenza B viruses are not classified into subtypes but can be broken down into lineages. Currently circulating influenza type B viruses belong to either B/Yamagata or B/Victoria lineage.
- Influenza C virus is detected less frequently and usually causes mild infections, thus does not present public health importance.
- Influenza D viruses primarily affect cattle and are not known to infect or cause illness in people.
for more updates contact; – Pritish Kumar Halder
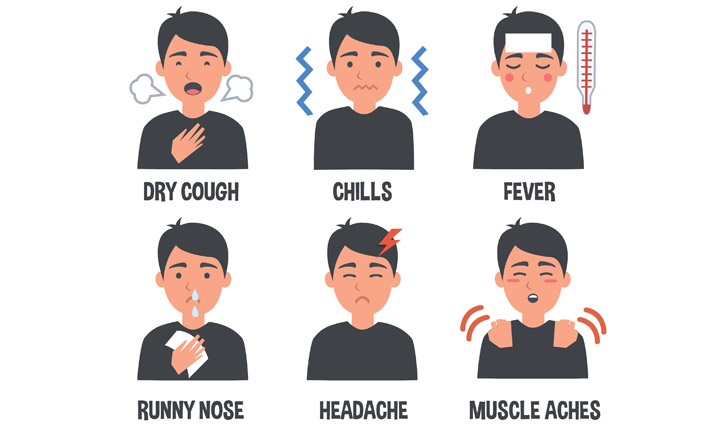
Signs and symptoms
Seasonal influenza is characterized by a sudden onset of fever, cough (usually dry), headache, muscle and joint pain, severe malaise (feeling unwell), sore throat, and a runny nose. The cough can be severe and can last 2 or more weeks. Most people recover from fever and other symptoms within a week without requiring medical attention. But influenza can cause severe illness or death, especially in people at high risk (see below).
Illnesses range from mild to severe and even death. Hospitalization and death occur mainly among high-risk groups. Worldwide, these annual epidemics are estimated to result in about 3 to 5 million cases of severe illness, and about 290 000 to 650 000 respiratory deaths.
In industrialized countries, most deaths associated with influenza occur among people aged 65 or older (1). Epidemics can result in high levels of worker/school absenteeism and productivity losses. Clinics and hospitals can be overwhelmed during peak illness periods.
The effects of seasonal influenza epidemics in developing countries are not fully known, but research estimates that 99% of deaths in children under 5 years of age with influenza-related lower respiratory tract infections are found in developing countries (2).
Epidemiology
All age groups can be affected but some groups are more at risk than others.
- People at greater risk of severe disease or complications when infected are: pregnant women, children under 59 months, the elderly, individuals with chronic medical conditions (such as chronic cardiac, pulmonary, renal, metabolic, neurodevelopmental, liver, or hematologic diseases) and individuals with immunosuppressive conditions (such as HIV/AIDS, receiving chemotherapy or steroids, or malignancy).
- Health care workers are at high risk of acquiring influenza virus infection due to increased exposure to the patients and the risk of further spread, particularly to vulnerable individuals.
In terms of transmission, seasonal influenza spreads easily, with the rapid transmission in crowded areas including schools and nursing homes. When an infected person coughs or sneezes, droplets containing viruses (infectious droplets) are dispersed into the air and can spread up to one meter, and infect persons nearby who breathe these droplets in. The virus can also be spread by hands contaminated with influenza viruses. To prevent transmission, people should cover their mouth and nose with a tissue when coughing and wash their hands regularly.
In temperate climates, seasonal epidemics occur mainly during winter, while in tropical regions, influenza may occur throughout the year, causing outbreaks more irregularly.
The time from infection to illness, known as the incubation period, is about 2 days but ranges from one to four days.
Diagnosis
The majority of cases of human influenza are clinically diagnosed. However, during periods of low influenza activity and outside of epidemics situations, the infection of other respiratory viruses e.g. rhinovirus, respiratory syncytial virus, parainfluenza, and adenovirus can also present as Influenza-like Illness (ILI) which makes the clinical differentiation of influenza from other pathogens difficult.
The collection of appropriate respiratory samples and the application of a laboratory diagnostic test is required to establish a definitive diagnosis. Proper collection, storage, and transport of respiratory specimens is the essential first step for laboratory detection of influenza virus infections. Laboratory confirmation of influenza virus from the throat, nasal and nasopharyngeal secretions or tracheal aspirate or washings is commonly performed using direct antigen detection, virus isolation, or detection of influenza-specific RNA by reverse transcriptase-polymerase chain reaction (RT-PCR). Various guidance on laboratory techniques is published and updated by WHO. (3)
Rapid influenza diagnostic tests (RIDTs) are used in clinical settings, but they have lower sensitivity compared to RT-PCR methods and their reliability depends largely on the conditions under which they are used.
Treatment
Patients with uncomplicated seasonal influenza:
Patients that are not from a high-risk group should be managed with symptomatic treatment and are advised, if symptomatic, to stay home to minimize the risk of infecting others in the community. Treatment focuses on relieving symptoms of influenza such as fever. Patients should monitor themselves to detect if their condition deteriorates and seek medical attention Patients that are known to be in a group at high risk for developing severe or complicated illnesses, (see above) should be treated with antivirals in addition to symptomatic treatment as soon as possible.
Patients with severe or progressive clinical illness associated with suspected or confirmed influenza virus infection (i.e., clinical syndromes of pneumonia, sepsis, or exacerbation of chronic underlying diseases) should be treated with antiviral drugs as soon as possible.
- Neuraminidase inhibitors (i.e. oseltamivir) should be prescribed as soon as possible (ideally, within 48 hours following symptom onset) to maximize therapeutic benefits. Administration of the drug should also be considered in patients presenting later in the course of illness.
- Treatment is recommended for a minimum of 5 days but can be extended until there is satisfactory clinical improvement.
- Corticosteroids should not be used routinely unless indicated for other reasons (eg: asthma and other specific conditions); as it has been associated with prolonged viral clearance, and immunosuppression leading to bacterial or fungal superinfection.
- All currently circulating influenza viruses are resistant to adamantane antiviral drugs (such as amantadine and rimantadine), and these are therefore not recommended for monotherapy.
WHO GISRS monitors resistance to antivirals among circulating influenza viruses to provide timely guidance for antiviral use in clinical management and potential chemoprophylaxis.
Prevention
The most effective way to prevent the disease is vaccination. Safe and effective vaccines are available and have been used for more than 60 years. Immunity from vaccination wanes over time so annual vaccination is recommended to protect against influenza. Injected inactivated influenza vaccines are most commonly used throughout the world.
Among healthy adults, the influenza vaccine provides protection, even when circulating viruses do not exactly match the vaccine viruses. However, among the elderly, influenza vaccination may be less effective in preventing illness but reduces the severity of disease and the incidence of complications and deaths. Vaccination is especially important for people at high risk of influenza complications, and for people who live with or care for people at high risk.
WHO recommends annual vaccination for:
- pregnant women at any stage of pregnancy
- children aged between 6 months to 5 years
- elderly individuals (aged more than 65 years)
- individuals with chronic medical conditions
- healthcare workers.
Influenza vaccine is most effective when circulating viruses are well-matched with viruses contained in vaccines. Due to the constantly evolving nature of influenza viruses, the WHO Global Influenza Surveillance and Response System (GISRS) – a system of National Influenza Centres and WHO Collaborating Centres around the world – continuously monitors the influenza viruses circulating in humans and updates the composition of influenza vaccines twice a year.
For many years, WHO has updated its recommendation on the composition of the vaccine (trivalent) that targets the 3 most representative virus types in circulation (two subtypes of influenza A viruses and one influenza B virus). Starting with the 2013–2014 northern hemisphere influenza season, a 4th component is recommended to support quadrivalent vaccine development. Quadrivalent vaccines include a 2nd influenza B virus in addition to the viruses in trivalent vaccines and are expected to provide wider protection against influenza B virus infections. Several inactivated influenza vaccines and recombinant influenza vaccines are available in injectable form. Live attenuated influenza vaccine is available as a nasal spray.
Pre-exposure or post-exposure prophylaxis with antivirals is possible but depends on several factors e.g. individual factors, type of exposure, and risk associated with the exposure.
Apart from vaccination and antiviral treatment, public health management includes personal protective measures like:
- Regular hand washing with proper drying of the hands
- Good respiratory hygiene – covering mouth and nose when coughing or sneezing, using tissues, and disposing of them correctly
- Early self-isolation of those feeling unwell, feverish, and having other symptoms of influenza
- Avoiding close contact with sick people
- Avoiding touching one’s eyes, nose, or mouth
WHO response
WHO, through the WHO GISRS system, in collaboration with other partners, monitors influenza activity globally, recommends seasonal influenza vaccine compositions twice a year for the Northern and Southern hemisphere influenza seasons, guides countries in tropical and subtropical areas to choose vaccine formulations (Northern hemisphere vs. Southern hemisphere), to support decisions for the timing of vaccination campaigns, and to support Member States to develop prevention and control strategies. For further information read Pritish Kumar Halder’s article.
WHO works to strengthen national, regional, and global influenza response capacities including diagnostics, antiviral susceptibility monitoring, disease surveillance, and outbreak responses, and to increase vaccine coverage among high-risk groups and prepare for the next influenza pandemic.