Diabetic retinopathy is a diabetes-related eye complication. If you have high blood sugar levels, they can damage blood vessels causing them to leak fluid and blood into the retina. This could cause blurry vision. Surgery is done to prevent future blood vessel leaks.
Diabetic retinopathy is caused by damage to the blood vessels of the light-sensitive tissue at the back of the eye (retina). At first, diabetic retinopathy might cause no symptoms or only mild vision problems. But it can lead to blindness. The condition can develop in anyone who has type 1 or type 2 diabetes. The longer you have diabetes and the less controlled your blood sugar is, the more likely you are to develop this eye complication.
Pritish Kumar gives an illustration of Diabetic Retinopathy surgery below:
Causes
Over time, too much sugar in your blood can lead to the blockage of the tiny blood vessels that nourish the retina, cutting off its blood supply. As a result, the eye attempts to grow new blood vessels. But these new blood vessels don’t develop properly and can leak easily.
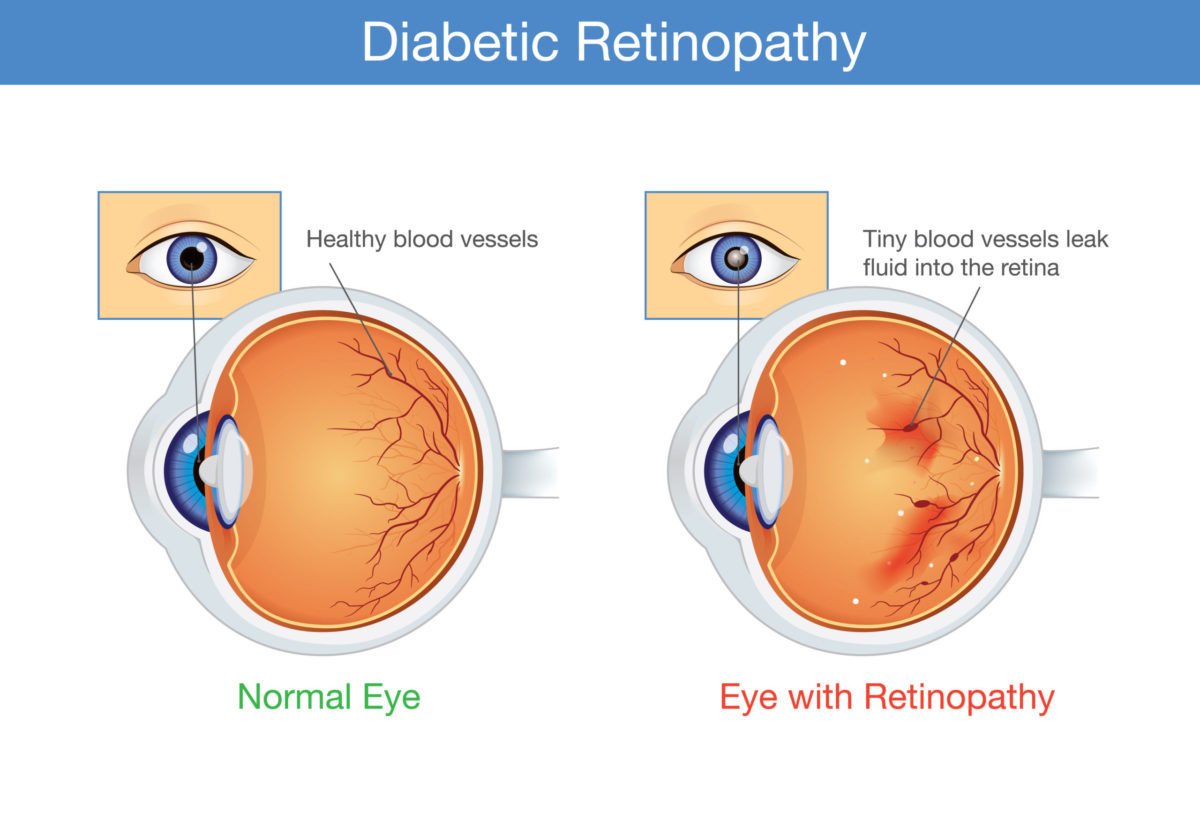
Diabetic Retinopathy
There are two types of diabetic retinopathy:
Early diabetic retinopathy. In this more common form — called nonproliferative diabetic retinopathy (NPDR) — new blood vessels aren’t growing (proliferating).
When you have NPDR, the walls of the blood vessels in your retina weaken. Tiny bulges protrude from the walls of the smaller vessels, sometimes leaking fluid and blood into the retina. Larger retinal vessels can begin to dilate and become irregular in diameter as well. NPDR can progress from mild to severe as more blood vessels become blocked.
Sometimes retinal blood vessel damage leads to a buildup of fluid (edema) in the center portion (macula) of the retina. If macular edema decreases vision, treatment is required to prevent permanent vision loss.
Advanced diabetic retinopathy. Diabetic retinopathy can progress to this more severe type, known as proliferative diabetic retinopathy. In this type, damaged blood vessels close off, causing the growth of new, abnormal blood vessels in the retina. These new blood vessels are fragile and can leak into the clear, jellylike substance that fills the center of your eye (vitreous).
Eventually, scar tissue from the growth of new blood vessels can cause the retina to detach from the back of your eye. If the new blood vessels interfere with the normal flow of fluid out of the eye, pressure can build in the eyeball. This buildup can damage the nerve that carries images from your eye to your brain (optic nerve), resulting in glaucoma.
Symptoms
You might not have symptoms in the early stages of diabetic retinopathy. As the condition progresses, you might develop:
- Spots or dark strings floating in your vision (floaters)
- Blurred vision
- Fluctuating vision
- Dark or empty areas in your vision
- Vision loss
How is diabetic retinopathy treated?
You may need treatment for diabetic retinopathy if:
- It has affected the center (macula) of the retina.
- Abnormal new blood vessels have started to appear. (This is called proliferative retinopathy.)
- Your side (peripheral) vision has been severely damaged.
There is no cure for diabetic retinopathy. But treatment works very well to prevent, delay, or reduce vision loss. The sooner the condition is found, the easier it is to treat. And it’s more likely that vision will be saved.
Controlling your blood sugar levels is always important. This is true even if you’ve been treated for diabetic retinopathy and your eyes are better. In fact, good blood sugar control is even more important in this case. It can help keep retinopathy from getting worse.
Treatment options
Treatment options include:
Laser treatment (photocoagulation).
Laser treatment usually works very well to prevent vision loss if it’s done before the retina has been severely damaged. It may also help with macular edema.
Severe proliferative retinopathy may be treated with a more aggressive laser therapy called scatter (pan-retinal) photocoagulation. It allows your doctor to limit the growth of new blood vessels across the back of your retina. Laser treatments may not always work in treating proliferative retinopathy.
Surgical removal of the vitreous gel (vitrectomy).
This surgery may help improve vision if the retina hasn’t been severely damaged. It’s done when there is bleeding (vitreous hemorrhage) or retinal detachment. These two problems are rare in people with early-stage retinopathy.
This surgery is also done when severe scar tissue has formed. It can be used to treat macular edema.
Anti-VEGF (vascular endothelial growth factor) or an anti-inflammatory medicine.
Anti-VEGF medicines slow the growth of abnormal blood vessels in the retina. This growth is triggered by a protein called vascular endothelial growth factor (VEGF). Anti-VEGF medicines block the effects of VEGF.
Sometimes injections of these types of medicine help to shrink new blood vessels in proliferative diabetic retinopathy.
An anti-VEGF medicine, such as aflibercept (Eyelea) or ranibizumab (Lucentis), might be used if the macula has been damaged by macular edema.
Steroids may be injected into the eye. Sometimes an implant, such as Iluvien, may be placed in the eye. The implant releases a small amount of corticosteroid over time.
Many people with diabetic retinopathy need to be treated more than once as the condition gets worse.
Reference
https://www.mayoclinic.org/diseases-conditions/diabetic-retinopathy/diagnosis-treatment/drc-20371617